Thyroid Related Eye Disease
Thyroid Eye Disease (TED) Graves' Ophthalmopathy disease could present clinically with one of the following characteristic signs:

- exophthalmos (protuberance of one or both eyes)
- a non-pitting edema (pretibial myxedema), with thickening of the skin usually found on the lower extremities
- fatigue, weight loss with increased appetite, and other symptoms of hyperthyroidism
- rapid heart beats
- muscular weakness
- The two signs that are truly 'diagnostic' of Graves' disease (i.e., not seen in other hyperthyroid conditions) are exophthalmos and non-pitting edema (pretibial myxedema). Goiter is an enlarged thyroid gland and is of the diffuse type (i.e., spread throughout the gland). Diffuse goiter could be seen with other causes of hyperthyroidism, although Graves' disease is the most common cause of diffuse goiter. A large goiter will be visible to the naked eye, but a smaller goiter (very mild enlargement of the gland) could be detectable only by physical exam. Occasionally, goiter is not clinically detectable but could be seen only with CT or ultrasound examination of the thyroid.
- Normothyroidism is also seen, and occasionally also hypothyroidism, which could assist in causing goiter (though it is not the cause of the Graves disease). Hyperthyroidism in Graves' disease is confirmed, as with any other cause of hyperthyroidism, by measuring elevated blood levels of free (unbound) T3 and T4.
- Other useful laboratory measurements in Graves' disease include thyroid-stimulating hormone (TSH, usually low in Graves' disease due to negative feedback from the elevated T3 and T4), and protein-bound iodine (elevated). Thyroid-stimulating antibodies could also be detected serologically.
- Biopsy to obtain histiological testing is not normally required but could be obtained if thyroidectomy is performed.
- Differentiating two common forms of hyperthyroidism such as Graves' disease and Toxic multinodular goiter is important to determine proper treatment. Measuring TSH-receptor antibodies with the h-TBII assay has been proven efficient and was the most practical approach found in one study.
Thyroid Eye disease
- Thyroid-associated ophthalmopathy is one of the most typical symptoms of Graves' disease. It is known by a variety of terms, the most common being Graves' ophthalmopathy. Thyroid eye disease is an inflammatory condition, which affects the orbital contents including the extraocular muscles and orbital fat. It is almost always associated with Graves' disease but could rarely be seen in Hashimoto's thyroiditis, primary hypothyroidism, or thyroid cancer.
- The ocular manifestations that are relatively specific to Grave's disease include soft tissue inflammation, proptosis (protrusion of one or both globes of the eyes), corneal exposure, and optic nerve compression. Also seen, if the patient is hyperthyroid, (i.e., has too much thryoid hormone) are more general manifestations, which are due to hyperthyroidism itself and which could be seen in any conditions that cause hyperthyroidism (such as toxic multinodular goiter or even thyroid poisoning). These more general symptoms include lid retraction, lid lag, and a delay in the downward excursion of the upper eyelid, during downward gaze.
- It is believed that fibroblasts in the orbital tissues could express the Thyroid Stimulating Hormone receptor (TSHr). This could explain why one autoantibody to the TSHr can cause disease in both the thyroid and the eyes
Eye Problems In Thyroid Eye Disease

- The primary problem that is seen with the eyes in Grave’s disease is the inflammation of fat and muscle tissue that is located behind the eye. Due to this, the eye is pushed forward, giving the appearance of larger than normal eyes. This is called exophthalmos.
- The spectrum of eye problems seen with Grave’s disease is called Grave’s ophthalmopathy. However, it must be borne in mind that Hashimoto’s thyroiditis and thyroid cancer can sometime cause similar eye problems.
- Some of the common problems associated with Grave’s ophthalmopathy include –
Corneal disease
-
- As the eye is bulged forwards, the upper eyelid fails to cover the entire eye to moisten it with secretions from the lacrimal gland. Due to this, the cornea, which is the part of the eye exposed to the surrounding atmosphere, can get dry.
- A dry cornea can make blinking difficult and patients may experience a gritty sensation. This can lead to either completely dry eyes, or sometimes make the eyes water excessively as a protective mechanism.
- A dry and exposed cornea also makes it prone to getting infected. Ulcers may form on the cornea which can sometimes be very painful and can lead to blurred vision.
Lid Retraction
Increased pressure around the eyes
- With the expansion and inflammation of tissues at the back of the eye, the increased pressure that develops pushes the eyeball forward even further.
- This can make the eye painful, especially on movement of the eyes. Associated with this is an intense headache which also worsens when the eyes are moved.
- The excessive pressure on the eyeball can also lead to blurred vision.
Proptosis
- The bulging of the eyeballs is called proptosis. Proptosis can be cosmetically unpleasant and makes patients very wary of how their eyes look.

- Proptosis leads to what is called a ‘staring’ look. This is where the pupils and iris are clearly seen, along with a large portion of the ‘white’ of the eyeball. Some people compare it to a ‘startled’ look.
Strabismus and Double vision
-
- Strabismus is the medical term for squint. Due to the pushing of the eyeballs out of the socket, the position of the eyeball may not be symmetrical to each other.
- In other words, the eyes may not bulge out in a straight manner. Furthermore, the excessive tissue behind the eyeball makes eye movements harder and more restricted.
- This restricted movement can lead to a squint (strabismus) along with double vision
Optic neuropathy
-
- The optic nerve is the nerve that is responsible for transmitting images that we see in the form of electrical signals to the brain. It is located at the back of the eye and is surrounded by fat tissue and muscle.
- In advanced cases of Grave’s disease, the excessive fat and muscle tissue growth behind the eyeball can place a great deal of pressure on the optic nerve. This compression of the nerve can lead to a condition called optic neuropathy.
- Optic neuropathy causes blurred vision, and in rare cases can lead to irreversible blindness.
Other symptoms
Some other symptoms that patients with thyroid eye disease may experience include lid tremor (when eyes are closed), infrequent blinking, difficulty eversing the eyelid and decreased forehead wrinkling.
Thyroid Eye Disease in detail
- Grave's Ophthalmolopathy is the most common caused of unilateral or bilateral proptosis in adults.
- It commonly occurs between the ages of 25-50, although it could also present in adolescents.
- Diagnosis is made based on clinical findings including proptosis, eyelid retraction, restrictive myopathy and possibly compressive optic neuropathy. It is often grouped into two independent manifestations of this syndrome:
- Type I and Type II orbitapathy, but could overlap
More frequent signs:
|
Less frequent signs: |
- lid lag (upper and lower)
- exophthalmos
- diplopia
- lid edema
- chemosis
- conj injection over recti
- increased IOP with elevation
- keratopathy
|
- closed lid tremor
- infrequent blinking
- difficult eversion upper lid
- bruit over eye
- decrease forehead wrinkling with upgaze
- increased hippus
- pigmented lids
|
Werner's Classification
NO SPECS, with each class in four grades 0-4, a, b, c: mild to severe
-
- 0 No S/S
- 1 Only signs (lid retraction)
- 2 Soft tissue involved (chemosis, grit, etc)
- 3 Proptosis (min 28)
- 4 EOM involved
- 5 Corneal involvement
- 6 Sight loss
| Symptom |
Type I |
Type II |
| Sex predilection |
Female |
|
| Proptosis |
Symmetric |
Unilateral or bilateral |
| Eyelid retraction |
Symmetric |
Unilateral or bilateral |
| Orbital inflammation |
Minimal |
|
| Extraocular muscle inflammation/ restriction |
Minimal |
Frequent |
| Chemosis |
Unusual |
Usual |
| diplopia |
Unusual |
Frequent |
| Compressive optic neuropathy |
Unusual |
Frequent |
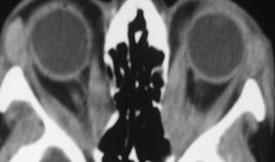
- Diagnosis is made on these clinical findings and could be confirmed on CT which shows enlargement of multiple extraocular muscles most commonly the inferior and medial rectus.
Systemic thyroid could be hyperthyroid, hypothyroid, or euthyroid. Treatment could include topical lubrication, systemic steroids, orbital decompression surgery, extraocular muscle adjustment, eyelid recession surgery and radiation therapy.
Radiological Findings
Diagnosis of Thyroid Eye Disease
- Thyroid eye disease can be diagnosed from clinical examination. A thyroid function test can confirm the presence of Grave’s disease.
- A CT scan of the orbit may show inflamed and enlarged tissues behind the eye. An MRI scan may also be useful.
Treatment of Thyroid Eye Disease
There are some simple measures that can be taken to help treat thyroid eye disease.
Medical treatment
- Applying a cool pack can soothe the eyes as the moisture can provide a degree of relief. Wearing protective sunglasses is important as excessive exposure of the cornea of the eye to sunlight can lead to problems with vision.
- As dryness of eyes is a common problem, ophthalmologists often prescribe lubricating eye drops. These can keep the eyes moist and prevent the grittiness experienced when blinking.
- Facial swelling is a common problem that can be avoided by elevating the head end of the bed when sleeping. Swelling can also be treated with the help of steroids eye drops.
- Prescription glasses with prisms may help some people with double vision.
Surgical treatment
- There are different surgical procedures that could help patients with thyroid eye disease.
- As previously noted, lid lag is a common problem leaving a large part of the cornea exposed. Repositioning the eyelid can prevent over-exposure of the cornea, preventing ulcer formation.
- Muscle infiltration that is seen in Grave’s ophthalmopathy can lead to scarring as time passes. Scarring makes the eye muscles shorter than normal, prohibiting smooth eye movements. As time passes, this can lead to double vision. Surgical resection of these muscles and reattachment to allow better movement and easy reading is often done to treat this problem.
- In advanced cases of eye disease when eyesight itself is threatened, orbital decompression surgery is necessary. Here, the eye socket bone (orbit) is removed so as to allow extra space from the sinuses for eye movements. As time passes, the vision improves as there is more room for the swollen tissues to sit and for the eye to move. However, this surgery does bear certain risks of double vision in rare cases.
- Always ensure that all surgical procedures are performed after the risks and benefits have been explained by expert ophthalmologists.
Prevention
- There are no specific preventive measures to avoid thyroid eye disease. However, when treatments are ongoing for Grave’s disease, steps may be taken to prevent eye disease from getting any worse.
- For example, if radio-iodine therapy is being prescribed, there is always a chance that eye disease could worsen. Co-prescribing steroids could help prevent this.
- Stopping smoking can prevent worsening of eye disease.